 iStockphoto/Thinkstock
iStockphoto/Thinkstock
The relationship between autoimmunity and lymphoma may become clearer with the study of autoimmune lymphoproliferative syndrome, or ALPS, according to the American Autoimmune Related Diseases Organization.
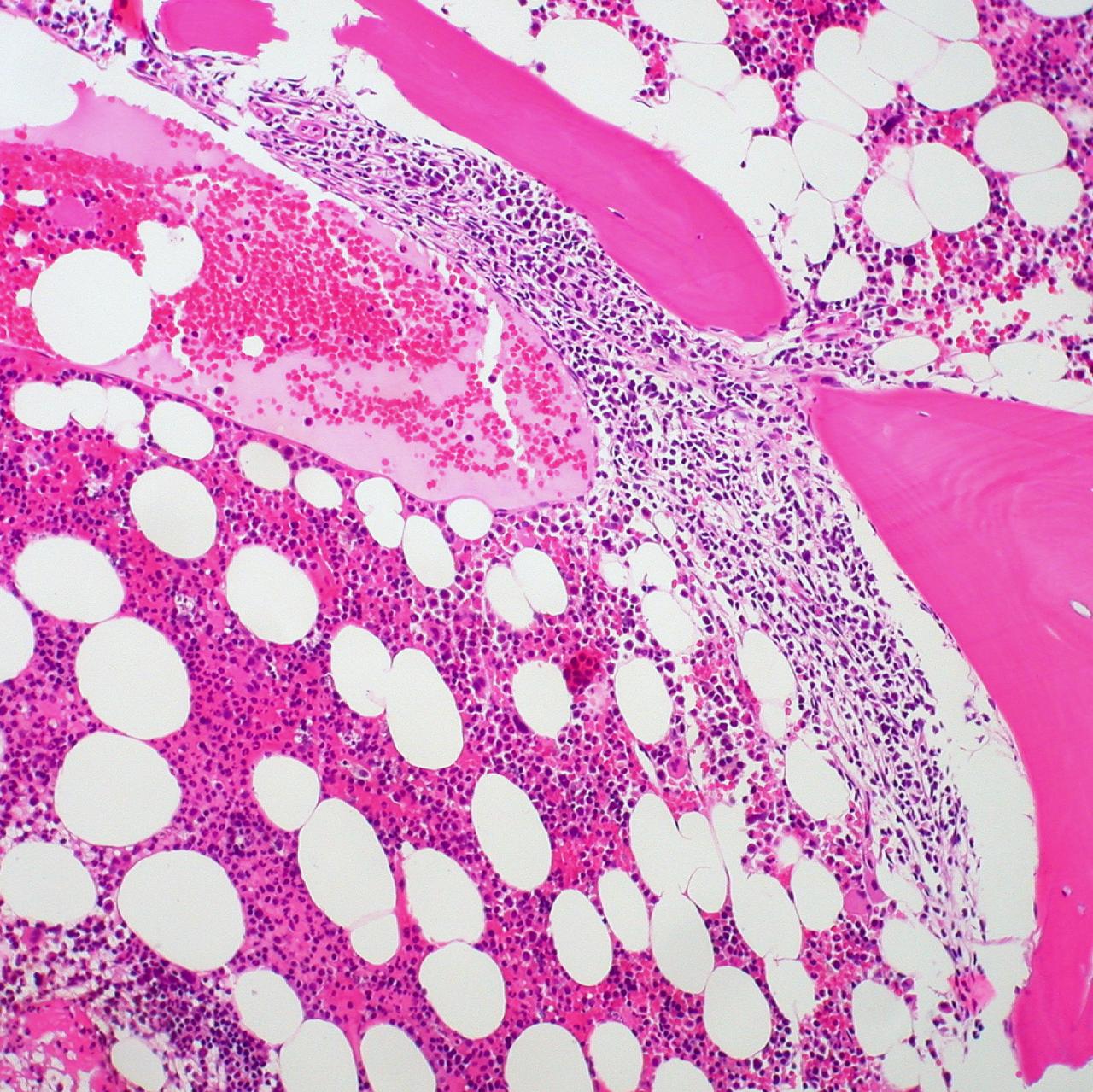
Their website reported that ALPS is a recently described disease entity, associated with a mutation in one of the genes that regulates death of white blood cells (lymphocytes).
The National Institute of Allergy and Infectious Diseases provided a detailed description of ALPS. Symptoms include fatigue, bruising, and nose bleeds. Little red spots called petechiae may show up on the skin, and some patients have skin rashes.
The spleen, lymph nodes, and liver may be enlarged. The condition usually shows up during childhood, but adults can also develop it.
Unlike lymphoma, ALPS is not cancer and does not get worse with time. Patients diagnosed as children often improve as they become teenagers and adults.
The degree of illness in ALPS ranges from mild to severe. Patients may be susceptible to bacterial infection, and may have autoimmune damage to almost any organ. ALPS is not contagious.
The genetic mutations responsible for ALPS can occur spontaneously. They can also be inherited, so family history is a risk factor.
Steroids are the primary treatment for ALPS. The risks of long-term steroid treatment include weight gain, elevated blood sugar, thinning of the bones, poor wound healing, difficulty in fighting infections, mood swings, and cataracts. Other drugs such as mycophenolate mofetil can be used to limit the side effects of steroids.
Other treatments included vaccinations to prevent infectious disease, and blood transfusions to treat anemia. Surgery to remove the spleen may be beneficial for patients with severe disease that does not respond to drug treatment.
Joao B. Oliveira of the National Institutes of Health (NIH) and colleagues provided a review of how ALPS is diagnosed. “Lymphadenopahy in children for which no infectious or malignant cause can be ascertained constitutes a challenging diagnostic dilemma,” Olivereira wrote.
Investigators at the NIH suggested criteria to diagnose ALPS in 1999, and updated these recommendations in the fall of 2009. The diagnosis is now based on specific blood tests as well as symptoms and family history.
References:
American Autoimmune Related Diseases Organization. Patient Information. Web. May 3, 2012.
http://www.aarda.org/patient_information.php
National Institute of Allergy and Infectious Diseases. Autoimmune Lymphoproliferative Syndrome. Web. May 3, 2012.
http://www.niaid.nih.gov/topics/ALPS/understanding/Pages/whatIsAlps.aspx
Oliveira JB et al, “Revised diagnostic criteria and classification for the autoimmune lymphoproliferative syndrome (ALPS): report from the 2009 NIH International Workshop”, Blood. 2010 Oct 7; 116(14): e35-40.
http://www.ncbi.nlm.nih.gov/pubmed/20538792
Reviewed April 4, 2012
by Michele Blacksberg RN



Add a CommentComments
There are no comments yet. Be the first one and get the conversation started!